A Review on Complement Diagnostics
Volume 18, Issue 1, Jan 2023 (download full article in pdf)
Editorial note:
The complement system though commonly regarded as component of the innate immune system that protect our bodies from infection, it has increasingly evident that it has important roles in other immune surveillance and housekeeping functions, that it is involved in a wide and diverse range of clinical conditions. In this review, Dr Elaine Au provided an overview of the complement diagnostics and its clinical applications. We welcome any feedback or suggestions. Please direct them to Dr Elaine Au of Education Committee, the Hong Kong College of Pathologists. Opinions expressed are those of the authors or named individuals, and are not necessarily those of the Hong Kong College of Pathologists.
Dr Au Yuen Ling Elaine
Consultant, Division of Clinical Immunology, Department of Pathology, Queen Mary Hospital
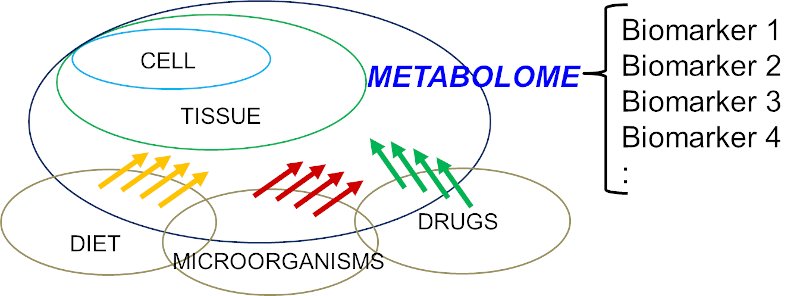
The complement system not only as part of the innate immune system that contributes to the elimination of pathogens, and promote inflammation, it also modulates the adaptive immune response. Though its primary role is in host defense, it also serves an important role in clearance of apoptotic cells and immune complexes. Low or dysregulated activity in complement system has been described in a range of disease and pathological conditions.
The Complement system
The complement system comprises approximately 50 proteins, that are found in fluid phase or bound to cell surface (2). The central complement reaction involves the cleavage of C3 into C3b and C3a, which is promoted by the C3 convertase. Collectively, there are three activation pathways forming the C3 convertase. The classical pathway (CP) is triggered by the immune complexes, while the lectin pathway (LP) is triggered by the binding of mannan-binding lectin (MBL) or ficolins to carbohydrates or pathogen-associated molecular patterns. Both activation of CP and LP would lead to the formation of C4b2a as C3 convertase. On the other hand, in the alternative pathway (AP), there is a constant low-grade hydrolysis of C3, that binds factor B and cleaves factor D to generate a fluid phase C3 convertase, that is self- limited in healthy state. However, the AP will be activated and amplified through binding of the cleaved C3 to pathogens or altered tissues. Hence, AP helps to amplify complement activation initiated from CP and LP. The pathways converge in a common pathway to form the membrane attack complex (C5b-9). In addition, the cleavage of C3 and C5 generates C3a and C5 a, that act as anaphylatoxins, while the target bound C3 fragments (C3b, iC3b, C3d, g) facilitate phagocytosis.
The complement activation is delicately controlled by multiple soluble and membrane bound regulators. Factor H, C4b binding protein, the membrane proteins complement receptor 1 CR1 (CD35), decay acceleration factor (CD55), and membrane cofactor protein MCP (CD46), act as cofactors for plasma proteinase factor I, accelerating the decay of convertases. In addition, CD59 and C1 inhibitor regulate the C5b-9 complex and the C1 complex respectively.
Examples of complement diagnostics indications and associated disease conditions
A broad spectrum of clinical conditions is associated with complement deficiencies or its overactivation / dysregulation. The clinical consequences can be broadly categorized into three areas. 1) susceptibility to infection, 2) autoimmunity and 3) defects in controlling and limiting complement activation.
Infection susceptibility
In general, complement deficiencies are associated with increased risk of infections, especially encapsulated bacterial infections, most commonly Pneumococci, Hemophilus etc. In particular, individuals suffering from deficiencies in the terminal components (C5-C9) or properdin are susceptible to Neisseria infections. Hence, complement studies are indicated in the workup of young individuals suffering from recurrent infections (e.g. recurrent sinopulmonary infections, meningitis, etc), especially in recurrent infections caused by encapsulated bacteria. Nevertheless, primary component deficiency is rare, and most of these conditions are autosomal recessive (X-linked inheritance in properdin deficiency) (1).
Autoimmune diseases
Deficiency in early components of the CP, is frequently associated with lupus like autoimmune conditions. The associations range from 10% prevalence of lupus like conditions in C2 deficiency, to C1r/s (57% prevalence), C4 (75% prevalence) and C1q (90% prevalence) (2). These deficiencies can be confirmed in genetic studies and components measurement. Overall, primary deficiency is relatively uncommon. More often, lupus and other autoimmune immune complex diseases causes secondary complement components deficiency as consumption due to the immune complex activation. The component levels, e.g. C3 and C4 levels, are commonly employed in the workup and disease activity monitoring in these conditions. In some occasions, measuring autoantibodies, such as anti-C1q antibody in hypocomplementemic urticarial vasculitis syndrome (HUVS) and lupus, is useful for diagnosis and prognostication.
C3 nephropathy and Thrombotic microangiopathy (TMA)
Uncontrolled AP activation may result in a number of kidney diseases and systemic conditions. C3 glomerulopathy comprises C3 glumoerulonephritis (C3GN) and dense-deposit disease (DDD), is a pathological condition defined by predominant C3 accumulation, with absent or scantly immunoglobulin deposition. Atypical post infectious glomerulonephritis also falls in the continuum of C3 GN and DDD (3). In these conditions, underlying predisposition, be it genetic or acquired, may not be clinically evident until a triggering event, such as infection or pregnancy, that unfold the complement dysregulation. Besides genetic predisposition, presence of autoantibodies, e.g. C3 nephritic factor (C3 Nef), anti-factor H, have been observed in some patients. C3Nef are autoantibodies that bind to components of AP convertase, prolonging its functional half-life, leading to continuous C3 activation and consumption, with lowish CP and AP studies. Factor H has important role in the regulation of complement activation. In some patients, they are predisposed to the disease due to Factor H dysfunction caued by mutation or anti-Factor H. Useful workup for C3 nephropathy includes the complement pathways, components and activation products studies, testing for plasma cells disorders, determination of autoantibodies (C3 Nef, anti-factor H), along with gene panel (C3, CFH, CFI, CFB, CFHR1-5) testing (3).
aHUS is a primary TMA, that is characterized by uncontrolled AP activation, presenting with microangiopathic hemolytic anaemia, thrombocytopenia and acute renal failure. The dysregulated AP could be caused by mutations of complement regulators, most commonly factor H, and in around 6-10% of cases, by the presence of anti- factor H (4). Initial workup includes investigations to exclude other co-existing medical conditions associated with HUS or other forms of TMA. Similar to the workup of C3GN, checking the complement pathways, components and activation products, along with anti-factor H and genetic testing (C3, CFH, CGI, CFB, MCP, CFHR1-5, THBD, DGKE) are useful.
TMA leads to generalized endothelial dysfunction, that can progress to multiorgan injury. Apart from primary causes, some disease or medical conditions may predispose to TMA. In particular transplant associated TMA (TA-TMA) has been an important clinical entity, that carries high mortality and morbidity. Recent literature has shown that complement pathway dysregulation may play a role in the process. The pathogenesis in TA-TMA is complex, that multifactorial factors contribute to the endothelial injury and pathological process. Complications related to transplant, including GVHD or infections, may also stimulate the complement pathways. Complement blockage therapy, e.g. eculizumab, is useful in managing complex cases. After workup to exclude other potential differential diagnoses, risk assessment is important. Although not all patients with TA-TMA will have elevated sC5b-9, patients with elevation are at increased risk of death from TA-TMA (5). Hence, the activation product measurement has been used as risk stratification for consideration of complement blockade therapy (4,6).
Paroxysmal Noctural Hemoglobuinuria (PNH)
PNH is a rare acquired disorder, that patients suffered from hemolysis with acute exacerbations, leading to anaemia, bone marrow failure and increased risk of thrombosis. PNH arises from an expanded clonal proliferation of hematopoietic cells with somatic mutations of the X chromosomal gene PIG-A. Lack of PIG-A resulted in inability to bind GPI-anchored proteins, including the membrane bound complement regulators, DAF and CD59. As a result, cells having the mutation are susceptible to complement mediated intravascular haemolysis. Assessing the surface expression of CD55 and CD59 is helpful for the diagnosis.
Inherited and Acquired C1 inhibitor deficiency
Hereditary angioedema (HAE) and acquired angioedema (AAE), are rare diseases caused by C1 inhibitor deficiency. As a result, unregulated bradykinin formation leads to angioedema. HAE is an autosomal dominant condition, with majority of cases suffered from reduced concentration (Type I) or less commonly, reduced function (Type II), of C1 inhibitor. Some patients may have similar clinical presentations as HAE cases, but as an acquired condition due to the presence of autoantibodies against C1 inhibitor. These patients usually presented at an older age, and may have underlying hematological malignancies or autoimmune conditions as predisposition. The diagnosis of HAE is based on C1 inhibitor and C4 measurement. It is important to include both antigenic and functional assays for C1 inhibitor, since around 15% of cases may have normal or elevated dysfunctional C1 inhibitor protein (Type II). Furthermore, serum C1q concentrations can be used to differentiate HAE from acquired angioedema (AAE) as the latter is characterized by decreased C1q antigen concentration and autoantibodies against C1-INH. Genetic analysis for SERPING1 variants status may also help in the workup.
Monitoring of Complement Regulatory Drugs
In recent years, drugs targeting complement activation has been in clinical use. Eculizumab is the first approved complement inhibitor, that it is a humanized monoclonal antibody that hinder C5 proteolytic activation, inhibit the generation of C5a and the initiation of the membrane attack complex C5b-9, through its binding to the C5. Eculizumab is approved in the treatment of PNH, aHUS and refractory myasthenia gravis. Complement studies, such as CH50/ AH 50, and activation products (sC5b-9), have been employed in the treatment monitoring (7). In some specialized laboratory, C5 function may also be tested. The best time to monitor the therapy is at trough, immediately before the next dose. With effective drug treatment, CH50/AH50 and C5 function will be low. The activation products will also be suppressed.
Complement assays
The assays used in complement assessment can be broadly divided into 1) screening assays of total functional complement activity, 2) quantification of individual components, 3) quantitation of activation products 4) detection of autoantibodies against the complement components 5) assessing cell surface expression or tissue deposition of complement proteins/ breakdown products, 6) genetic assays.
Apart from the rare primary component deficiency, complement is associated in a number of disease conditions (such as infections, sepsis, malignancy, immune complex diseases, etc) by activation via different pathways. When a component is activated in vivo, the component is taken up by receptors on leukocytes or Kupffer cells. This results in secondary deficiency as consumption. Note that in complement studies, some assays are sensitive to in-vitro activation. Consumption can also be an artifact from heat labile nature of the complement proteins combined with delayed freezing of specimen after sample collection. Overall, the specificity of single complement test is low. Assessing several markers of the pathways and careful interpretation of results as a whole, is useful. In some situations, complementary use of genetic tests may help in cases suspecting primary in nature.
Since EDTA is able to inhibit complement activation in vitro, it is commonly used for quantification of complement components, in particular for activation products. Since heparin and citrate are insufficient inhibitors of complement activation, these are not suitable. Serum, on the other hand, is used for complement function and autoantibodies assessment. Plasma and serum received for complement assays should be separated within 2 hours from collection and frozen at -70 degree Celsius (4). Careful attention to the pre analytical steps and storage is crucial in complement studies.
Screening assays for total functional complement activity
The main indication for total complement function screen is to detect complement deficiencies. Such deficiencies can be genetic (primary), acquired (secondary, e.g. to consumption after pathway activation), or as a consequence of treatment. These tests reflect the total amount of active complement component present in a freshly sampled serum, and reflect the potential of the serum sample to achieve full activation in vitro after addition of activator. The traditional assays used are CH50 and AH50, based on studying the lysis of antibody sensitized sheep erythrocytes (CH50 for the CP activity) and the lysis of untreated rabbit erythrocytes (AH50 for the AP activity). The lysis of erythrocytes correlates with the formation of the terminal membrane attack complex downstream of the pathways’ activation. The results are usually expressed as reciprocal dilutions of the sample required to produce 50% lysis. Besides the traditional assays, a variety of modified methods based on the hemolytic assay were done in different centers. The functional screen can also be tested by measuring the deposition of activation products (ELISA detecting C9 neoepitope generated in terminal complex formation) upon activation of the serum with immobilized complement activating substances on a microtiter plate. Targeted molecules for each pathway are coated in wells of the microtiter plates; Ig M for CP, mannan /acetylated bovine serum albumin for LP and LPS for AP. (8)
In general, the pathway screens may provide some hint to the underlying disease process. Absent/low AH50 with normal CH50 suggests alternative pathway component deficiency, while absent/low CH50 with normal AH 50 suggests early classical pathway components (C1, C2, C4) deficiency. Absent/low results in both AH50 and CH50 suggests a deficiency affecting common components (C3, C5, C6, C7, C8, C9) shared in both pathways or complement consumption. Further investigations, including quantitation of individual components, would be helpful. In the settings of multiple components deficiency, consumptive depletion is likely.
Quantitation of individual components
In cases where the screening assays indicating a complement deficiency, quantitation of individual components and interpreting the results as a profile is useful to further delineate the affected pathways and pathogenesis.
Measurement of complement components is commonly done by immunoprecipitation assays with polyclonal antibodies against the protein of choice, e.g. nephelometry and turbidimetry. Other assays, such as gel precipitation assays or enzyme immunoassays were also used. Overall, these assays are relatively robust, however, do not provide information on the conformation or activation status in vivo.
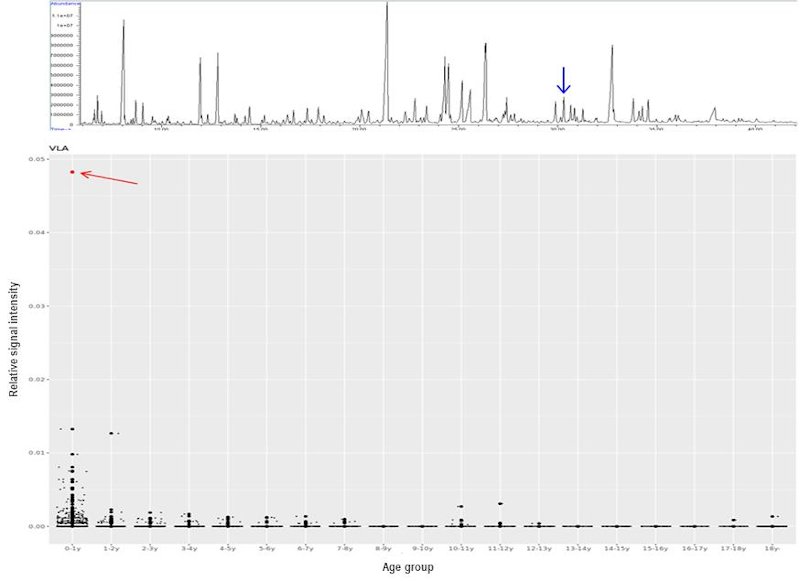
Quantitation of activation products
Abnormal total complement functional screen could be due to primary deficiency or deficiency secondary to consumptive loss. Measurement of individual components level is not able to distinguish between primary from secondary loss. On the other hand, in vivo complement activation in acute phase reaction may not always lead to low components measurement despite ongoing consumption. Hence, quantitation of activation products would be helpful in the assessment of complement activation. Among the activation products available for measurement, detection of the soluble form of the terminal complement complex (sC5b-9), is the most promising screen for complement activation. The terminal complex reflects the activation to the final stage of the three pathways. Moreover, sC5b-9 has a relatively long in vivo half-life (60 mins), compared to other activation products, and is more stable with respect to in vitro activation compared to early components fragments (1,4). Overall, these activation markers can be rapidly produced by complement activation in vitro, therefore, proper sample collection and handling is important.
Autoantibodies against complement components
Autoantibodies to complement components have been linked to a number of disease conditions. The pathogenesis is often caused by the dysregulation of complement activation, as in the case of C3NeF and anti-Factor H. Occasionally, it may be affecting non-complement pathway, as in the case of anti-C1 inhibitor related angioedema, that it is due to inefficient inhibition of the kallikrein-kinin system and bradykinin release (4).
Most often, these autoantibodies could be detected by enzyme immunoassays. Functional assays were also helpful in the assessment. For example, in C3 Nef detection, a hemolytic assay that utilizes unsensitized sheep erythrocytes, or assay detecting fluid-phase C3 conversion after incubation of patient serum with normal serum at 37degree Celsius, were commonly used for the C3 Nef activity detection (9).
Assessing cell surface expression or tissue deposition of complement proteins/ breakdown products
Measuring complement components and activation products directly on cell surface provides valuable information for the workup. For example, examining the deposition of various complement components in the glomeruli and peritubular capillary is useful for glomerulopathies assessment. Furthermore, studying the expression of membrane bound regulators is also helpful in some conditions, such as the use of flow cytometry assessment of CD55 and CD59 on blood cells in the diagnosis of PNH.
Genetic assays
With the advances in molecular diagnostics, complementary use of molecular diagnostics with traditional assays, has been increasingly employed in cases suspecting primary deficiency of complement factors or regulators. For example, gene panels study has been recommended in the workup of aHUS and C3 glomerulonephritis (3, 10-11).
Conclusion
With the vast and constantly growing knowledge in various disease process, along with expanding indications and emerging treatment options in complement mediated disorders, the application of complement diagnostics has been broadened and not limited to diagnosing rare primary genetic entities only. However, many of these assays remains highly subspecialized with limited availability, lack of standardization and complex interpretations. Careful standardization and close international collaborations and experience sharing, would be important for both the laboratory development and clinical applications in the field.
References
- Kirschfink M, Mollnes TE. Modern complement analysis. Clin Diagn Lab Immunol. 2003 Nov;10(6):982-9.
- Pickering MC, Botto M, Taylor PR, Lachmann PJ, Walport MJ. Systemic lupus erythematosus, complement deficiency, and apoptosis. Adv Immunol. 2000;76:227-324.
- Angioi A, Fervenza FC, Sethi S, Zhang Y, Smith RJ, Murray D, Van Praet J, Pani A, De Vriese AS. Diagnosis of complement alternative pathway disorders. Kidney Int. 2016 Feb;89(2):278-88.
- Ekdahl KN, Persson B, Mohlin C, Sandholm K, Skattum L, Nilsson B. Interpretation of Serological Complement Biomarkers in Disease. Front Immunol. 2018 Oct 24;9:2237.
- Jodele S, Davies SM, Lane A, Khoury J, Dandoy C, Goebel J, Myers K, Grimley M, Bleesing J, El-Bietar J, Wallace G, Chima RS, Paff Z, Laskin BL. Diagnostic and risk criteria for HSCT-associated thrombotic microangiopathy: a study in children and young adults. Blood. 2014 Jul 24;124(4):645-53.
- Jodele S, Dandoy CE, Lane A, Laskin BL, Teusink-Cross A, Myers KC, Wallace G, Nelson A, Bleesing J, Chima RS, Hirsch R, Ryan TD, Benoit S, Mizuno K, Warren M, Davies SM. Complement blockade for TA-TMA: lessons learned from a large pediatric cohort treated with eculizumab. Blood. 2020 Mar 26;135(13):1049-1057.
- Ricklin D, Barratt-Due A, Mollnes TE. Complement in clinical medicine: Clinical trials, case reports and therapy monitoring. Mol Immunol. 2017 Sep;89:10-21.
- Mollnes TE, Lea T, Frøland SS, Harboe M. Quantification of the terminal complement complex in human plasma by an enzyme-linked immunosorbent assay based on monoclonal antibodies against a neoantigen of the complex. Scand J Immunol. 1985 Aug;22(2):197-202.
- Nilsson B, Ekdahl KN. Complement diagnostics: concepts, indications, and practical guidelines. Clin Dev Immunol. 2012;2012:962702.
- Goodship TH, Cook HT, Fakhouri F, Fervenza FC, Frémeaux-Bacchi V, Kavanagh D, Nester CM, Noris M, Pickering MC, Rodríguez de Córdoba S, Roumenina LT, Sethi S, Smith RJ; Conference Participants. Atypical hemolytic uremic syndrome and C3 glomerulopathy: conclusions from a "Kidney Disease: Improving Global Outcomes" (KDIGO) Controversies Conference. Kidney Int. 2017 Mar;91(3):539-551.
- Loirat C, Fakhouri F, Ariceta G, Besbas N, Bitzan M, Bjerre A, Coppo R, Emma F, Johnson S, Karpman D, Landau D, Langman CB, Lapeyraque AL, Licht C, Nester C, Pecoraro C, Riedl M, van de Kar NC, Van de Walle J, Vivarelli M, Frémeaux-Bacchi V; HUS International. An international consensus approach to the management of atypical hemolytic uremic syndrome in children. Pediatr Nephrol. 2016 Jan;31(1):15-39.